Implementing and integrating new technology into patient care can be difficult at times, but with the right strategy, success is possible! Learn more about how a level IV NICU team was successful in developing an all-encompassing strategy to drive consistent utilization of transcutaneous monitoring with the goal of improving patient care.
The team identified 5 key areas that made their implementation successful:
 Make sure all your team members are informed and know their roles.
Make sure all your team members are informed and know their roles.
“Develop a training program that addresses all members of the neonatal team: nurses, respiratory therapists, neonatal nurse practitioners, and neonatologists.”
Why? Successful implementation of any technology relies on collective team knowledge. If only a few staff members receive training, gaps in understanding can lead to misuse or inconsistent application. Even if nurses aren’t responsible for managing the monitor or applying the sensor, they still need to know key details, such as not placing a diaper, tape, or swaddle over the sensor. Everyone has a role to play, and making sure everyone knows theirs and why it matters is key to successful implementation.
 Educate on the factors that influence correlation of tcpCO2 to PaCO2.
Educate on the factors that influence correlation of tcpCO2 to PaCO2.
The team identified 5 key areas that made their implementation successful:
 Make sure all your team members are informed and know their roles.
Make sure all your team members are informed and know their roles.
“Develop a training program that addresses all members of the neonatal team: nurses, respiratory therapists, neonatal nurse practitioners, and neonatologists.”
Why? Successful implementation of any technology relies on collective team knowledge. If only a few staff members receive training, gaps in understanding can lead to misuse or inconsistent application. Even if nurses aren’t responsible for managing the monitor or applying the sensor, they still need to know key details, such as not placing a diaper, tape, or swaddle over the sensor. Everyone has a role to play, and making sure everyone knows theirs and why it matters is key to successful implementation.
 Educate on the factors that influence correlation of tcpCO2 to PaCO2.
Educate on the factors that influence correlation of tcpCO2 to PaCO2.
“Drive a high level of competency about the relationship between perfusion, device calibration, site selection, and correlation.”
Why? Without an understanding of the factors influencing correlation, staff may have difficulty obtaining accurate readings, which can lead to skepticism about the technology’s reliability and hinder adoption. If tcpCO₂ readings don’t align with ABG values, clinicians may doubt the monitor’s effectiveness rather than recognizing and addressing potential causes. Thorough training empowers staff to prevent and troubleshoot discrepancies, supporting accurate readings and fostering confidence in transcutaneous monitoring across a wide range of patients.
 Develop trust in the technology.
Develop trust in the technology.
“Build broad trust in the technology by generating quality correlation data at the bedside with a review of proper blood sampling technique, and attention to detail with logging tcpCO2 values at the moment the blood draw is performed.”
Why? This one goes hand in hand with key area # 2. Once you have trained your team on how to get the best results from the monitor, document it and talk about it. Trust grows when clinicians see reliable data firsthand. By consistently reviewing and discussing tcpCO₂ readings alongside corresponding blood gas results — such as during rounds — teams gain confidence in the monitor’s accuracy. This trust paves the way for meaningful practice changes, like reducing the frequency of routine blood draws.
 Organize a proactive device maintenance program.
Organize a proactive device maintenance program.
“Establish “super users” and a proactive maintenance strategy to ensure monitors are always ready for use and to minimize time spent troubleshooting.”
Why? While transcutaneous monitors are user-friendly, they require regular upkeep, much like other technologies in the NICU. Designating a team of dedicated super users can ensure proper device care, efficient troubleshooting, and continuous readiness for patient use. A proactive maintenance plan, backed by a committed team, helps prevent disruptions and maximizes the monitor’s effectiveness in clinical practice.
 Don’t forget the “why” behind adopting transcutaneous technology.
Don’t forget the “why” behind adopting transcutaneous technology.
“Educate the entire team regarding the potential impact of fewer blood draws in relation to blood loss, pain, and infection, as well as the lung-protective value of titrated ventilatory care.”
Why? Your team is likely adopting transcutaneous monitoring to reduce the frequency of blood draws in the NICU and take a more proactive approach to protecting your patients’ developing brains and lungs. These are ambitious, important goals that require a team effort. Blood draws cause pain, which can contribute to longer-term developmental challenges, and lead to blood loss that may require transfusions. And, your patients’ tiny, vulnerable organs need every possible safeguard to support their growth and outcomes.
Ensuring your entire team understands the impact of transcutaneous monitoring and how it aligns with your NICU’s care goals is one of the most important steps toward successful implementation — for both your staff and, most importantly, your patients. When they understand the “why,” they’ll recognize how their use of the technology directly contributes to their patients’ outcomes.
Adopting new technology in any department comes with challenges — possibly even more so in the unpredictable and high-stakes environment of the NICU. However, by focusing on these five key areas, NICUs can successfully integrate transcutaneous monitoring and build their team’s confidence in using the technology. And that confidence is essential. When your team understands the technology and the impact it has, they feel empowered to use it to support patient care and improve outcomes for the tiniest, most vulnerable patients in the hospital.
“Drive a high level of competency about the relationship between perfusion, device calibration, site selection, and correlation.”
Why? Without an understanding of the factors influencing correlation, staff may have difficulty obtaining accurate readings, which can lead to skepticism about the technology’s reliability and hinder adoption. If tcpCO₂ readings don’t align with ABG values, clinicians may doubt the monitor’s effectiveness rather than recognizing and addressing potential causes. Thorough training empowers staff to prevent and troubleshoot discrepancies, supporting accurate readings and fostering confidence in transcutaneous monitoring across a wide range of patients.
 Develop trust in the technology.
Develop trust in the technology.
“Build broad trust in the technology by generating quality correlation data at the bedside with a review of proper blood sampling technique, and attention to detail with logging tcpCO2 values at the moment the blood draw is performed.”
Why? This one goes hand in hand with key area # 2. Once you have trained your team on how to get the best results from the monitor, document it and talk about it. Trust grows when clinicians see reliable data firsthand. By consistently reviewing and discussing tcpCO₂ readings alongside corresponding blood gas results — such as during rounds — teams gain confidence in the monitor’s accuracy. This trust paves the way for meaningful practice changes, like reducing the frequency of routine blood draws.
 Organize a proactive device maintenance program.
Organize a proactive device maintenance program.
“Establish “super users” and a proactive maintenance strategy to ensure monitors are always ready for use and to minimize time spent troubleshooting.”
Why? While transcutaneous monitors are user-friendly, they require regular upkeep, much like other technologies in the NICU. Designating a team of dedicated super users can ensure proper device care, efficient troubleshooting, and continuous readiness for patient use. A proactive maintenance plan, backed by a committed team, helps prevent disruptions and maximizes the monitor’s effectiveness in clinical practice.
 Don’t forget the “why” behind adopting transcutaneous technology.
Don’t forget the “why” behind adopting transcutaneous technology.
“Educate the entire team regarding the potential impact of fewer blood draws in relation to blood loss, pain, and infection, as well as the lung-protective value of titrated ventilatory care.”
Why? Your team is likely adopting transcutaneous monitoring to reduce the frequency of blood draws in the NICU and take a more proactive approach to protecting your patients’ developing brains and lungs. These are ambitious, important goals that require a team effort. Blood draws cause pain, which can contribute to longer-term developmental challenges, and lead to blood loss that may require transfusions. And, your patients’ tiny, vulnerable organs need every possible safeguard to support their growth and outcomes.
Ensuring your entire team understands the impact of transcutaneous monitoring and how it aligns with your NICU’s care goals is one of the most important steps toward successful implementation — for both your staff and, most importantly, your patients. When they understand the “why,” they’ll recognize how their use of the technology directly contributes to their patients’ outcomes.
Adopting new technology in any department comes with challenges — possibly even more so in the unpredictable and high-stakes environment of the NICU. However, by focusing on these five key areas, NICUs can successfully integrate transcutaneous monitoring and build their team’s confidence in using the technology. And that confidence is essential. When your team understands the technology and the impact it has, they feel empowered to use it to support patient care and improve outcomes for the tiniest, most vulnerable patients in the hospital.
Tools for your team
Implementation Planning Guide
Ready to take the next step in implementing transcutaneous monitoring in your unit? Use this implementation checklist to help your team stay organized and set up for success.
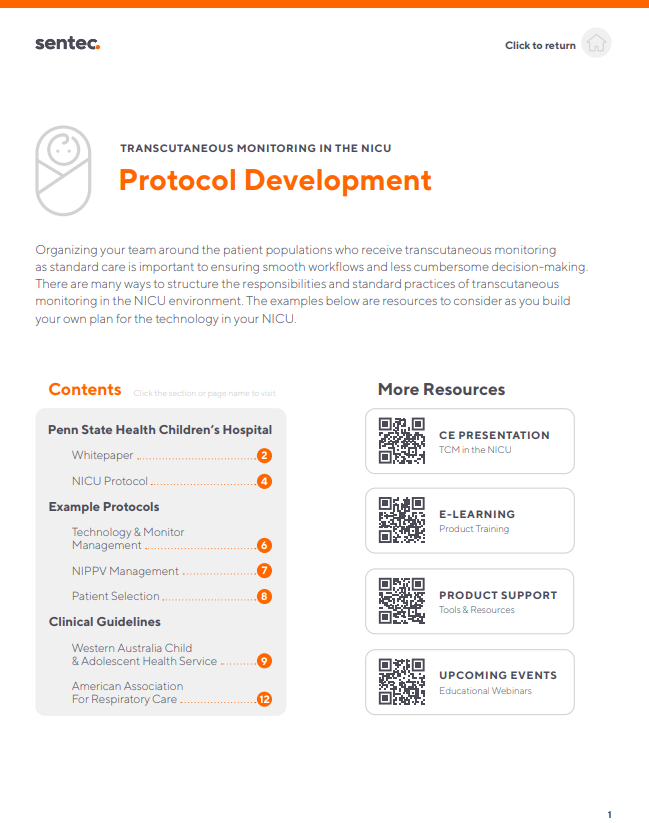
Protocol Development Packet
Once you have Sentec at the bedside, integrating the monitors into your protocols can help drive consistent use and maximize the benefits of transcutaneous monitoring. This resource provides example protocols from top-users of the technology.
Stay up-to-date with Sentec